
Newsroom
Radiotherapy and chemotherapy are widely practiced clinical applications with the ability to shape the tumor immune microenvironment, in which the cGAS-cGAMP-STING pathway plays a crucial role in augmenting anticancer immunity.
Studies have suggested that transferring cGAMP from tumor cells to infiltrating immune cells is a unique way to overcome the tumor cells’ lack of STING expression and elicit a robust type I interferon response. However, the precise mechanism underlying cGAMP’s cell-to-cell transfer within the tumor environment remains poorly understood.
In a study published in Science Immunology, Prof. XIAO Hui's team at the Shanghai Institute of Immunity and Infection (SIII) of the Chinese Academy of Sciences and Prof. LI Huabin's team from the Fudan University revealed a novel mechanism by which LRRC8/VRAC transports tumor-derived cGAMP into infiltrating immune cells to enhance the cytolytic functions of CD8 T cells and natural killer cells during radiotherapy and chemotherapy, providing new insight into cancer therapies.
Prof. XIAO's team has been focusing on deciphering the complex innate immune mechanisms against pathogens and cancers. The group has identified the Volume-Regulated Anion Channel LRRC8/VRAC as a bona fide cGAMP transporter, promoting the type I interferon response that is crucial for containing infections by herpes viruses, such as HSV-1.
In this study, the researchers revealed that the LRRC8A/C-containing VRAC channels played a vital role in mounting the anticancer immune responses to radiotherapy and chemotherapy. LRRC8/VRAC transferred cGAMP from irradiated cancer cells to infiltrating CD4 and CD8 T cells, thereby inducing a prominent type I interferon response that boosts the cytolytic effector functions of CD8 T cells and natural killer cells.
Moreover, the researchers demonstrated that T-cell receptor (TCR) activation by the cognate tumor antigen acted as a physiological signal to open the VRAC pore through PI(4,5)P2 and reactive oxygen species (ROS), allowing the rapid uptake of cGAMP and STING activation in mouse and human T cells. Tumor-derived extracellular ATP can act in synergy with TCR signaling to accelerate the transfer of extracellular cGAMP, which is sensitive to ENPP1 degradation.
The researchers further suggested that simultaneously inhibiting the extracellular ATP hydroxylase CD39 and the cGAMP hydroxylase ENPP1 can significantly enhance LRRC8/VRAC-mediated cGAMP transfer, leading to superior anticancer immunity.
"It is remarkable that we identify LRRC8/VRAC as a bona fide cGAMP transporter pivoting radiotherapy and chemotherapy’s anticancer efficacy. We believe that this finding could open up new avenues for future cancer immunotherapy bolstering T cell’s LRRC8/VRAC function," said Prof. XIAO.
This study demonstrates simultaneously boosting extracellular ATP and cGAMP as a novel approach to enhance the efficacy of radiotherapy, providing a proof-of-concept for harnessing in situ extracellular cGAMP to improve cancer therapy.
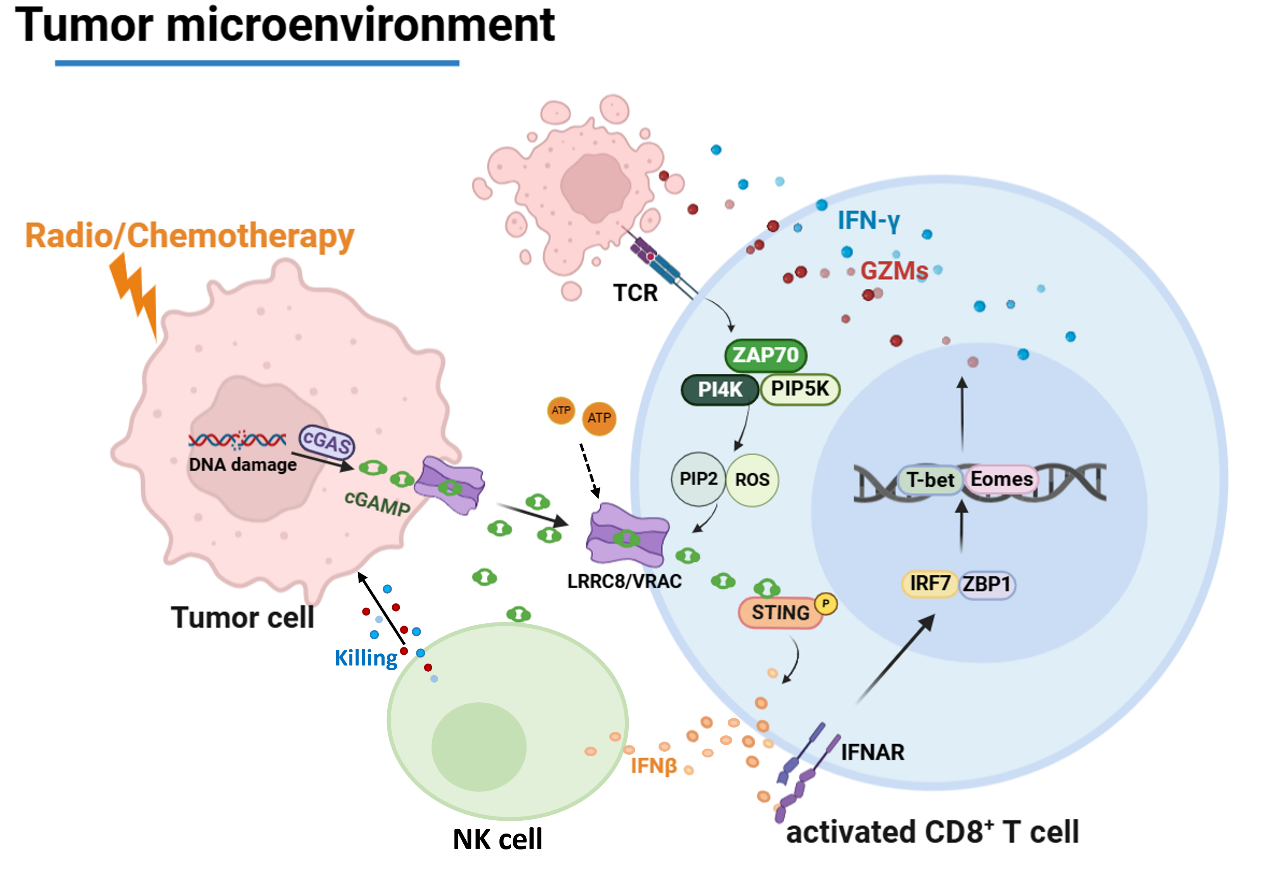
LRRC8/VRAC-mediated cGAMP transfer underlines radiotherapy and chemotherapy. (Image by SIII)
